 The liver is a vital organ responsible for detoxification, metabolism, and digestion, making its health crucial for overall well-being. If you’re dealing with issues within your liver, it can be
Read more
The liver is a vital organ responsible for detoxification, metabolism, and digestion, making its health crucial for overall well-being. If you’re dealing with issues within your liver, it can be
Read more
-
Liver Health: Preventive Measures and Lifestyle Changes to Support Liver Function
posted: Apr. 17, 2024.
 The liver is a vital organ responsible for detoxification, metabolism, and digestion, making its health crucial for overall well-being. If you’re dealing with issues within your liver, it can be
Read more
The liver is a vital organ responsible for detoxification, metabolism, and digestion, making its health crucial for overall well-being. If you’re dealing with issues within your liver, it can be
Read more
-
Ulcerative Colitis and Other Digestive Complications
posted: Apr. 01, 2024.
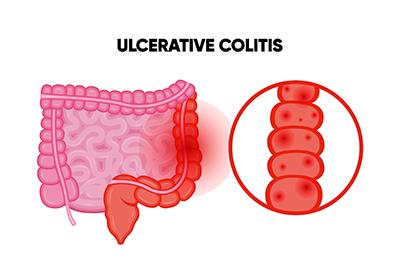 Digestive problems can affect your entire body. One of the most painful digestive conditions is ulcerative colitis, also known as inflammatory bowel disease or IBD. Your gastroenterologist is an expert
Read more
Digestive problems can affect your entire body. One of the most painful digestive conditions is ulcerative colitis, also known as inflammatory bowel disease or IBD. Your gastroenterologist is an expert
Read more
-
Treating Internal Hemorrhoids
posted: Mar. 18, 2024.
 Hemorrhoids are painful and embarrassing. They are also a subject most people don’t like to talk about. They are also a common problem. If you have hemorrhoids, you have a
Read more
Hemorrhoids are painful and embarrassing. They are also a subject most people don’t like to talk about. They are also a common problem. If you have hemorrhoids, you have a
Read more
-
Three Signs of GERD
posted: Mar. 01, 2024.
 Are you experiencing these symptoms of gastroesophageal reflux disease (GERD)?
Heartburn is something that everyone will inevitably experience. But what happens when heartburn keeps happening to you? This could signify a
Read more
Are you experiencing these symptoms of gastroesophageal reflux disease (GERD)?
Heartburn is something that everyone will inevitably experience. But what happens when heartburn keeps happening to you? This could signify a
Read more
-
Are You Dealing With Irritable Bowel Syndrome?
posted: Feb. 15, 2024.
 If you have frequent episodes of stomach or abdominal pain, it could be a sign of a serious gastrointestinal condition known as irritable bowel syndrome or IBS. Your gastroenterologist can
Read more
If you have frequent episodes of stomach or abdominal pain, it could be a sign of a serious gastrointestinal condition known as irritable bowel syndrome or IBS. Your gastroenterologist can
Read more
-
Colon Cancer Screening: Understanding Colonoscopies and Other Methods
posted: Feb. 01, 2024.
 Colon cancer can be deadly. In fact, it’s the third leading cause of cancer deaths, according to the American Cancer Society. Fortunately, colon cancer screening, available from your gastroenterologist, can
Read more
Colon cancer can be deadly. In fact, it’s the third leading cause of cancer deaths, according to the American Cancer Society. Fortunately, colon cancer screening, available from your gastroenterologist, can
Read more
-
Inflammatory Bowel Disease (IBD): Understanding Crohn's Disease and Ulcerative Colitis
posted: Jan. 16, 2024.
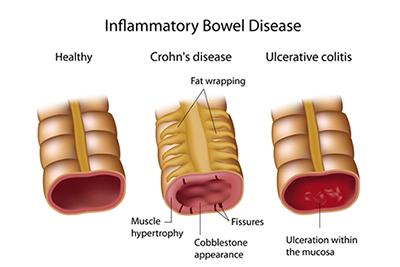 Inflammatory bowel disease (IBD) often relates to either Crohn’s disease or ulcerative colitis. Both conditions affect the gastrointestinal tract and cause chronic inflammation. When they aren’t treated, it can lead
Read more
Inflammatory bowel disease (IBD) often relates to either Crohn’s disease or ulcerative colitis. Both conditions affect the gastrointestinal tract and cause chronic inflammation. When they aren’t treated, it can lead
Read more
-
What Causes Acid Reflux?
posted: Jan. 01, 2024.
 Acid reflux, often termed heartburn or gastroesophageal reflux disease (GERD), occurs when stomach acid backs up into the esophagus. This backward flow can lead to a burning sensation in your
Read more
Acid reflux, often termed heartburn or gastroesophageal reflux disease (GERD), occurs when stomach acid backs up into the esophagus. This backward flow can lead to a burning sensation in your
Read more
-
Colon Cancer Screening FAQs
posted: Dec. 07, 2023.
 Colon cancer isn’t a topic people like to think about, but it’s important. Colon cancer may not show any signs or symptoms, but it can be deadly. Colon cancer screenings
Read more
Colon cancer isn’t a topic people like to think about, but it’s important. Colon cancer may not show any signs or symptoms, but it can be deadly. Colon cancer screenings
Read more
-
Don’t Ignore Your Acid Reflux
posted: Dec. 01, 2023.
 If you ever had a feeling of a burning liquid coming up to the back of your throat and pain in the upper chest area, you may have had a
Read more
If you ever had a feeling of a burning liquid coming up to the back of your throat and pain in the upper chest area, you may have had a
Read more
-
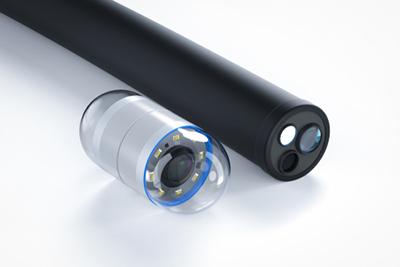
When Is an Endoscopy Needed?
posted: Nov. 10, 2023.
 When you’re dealing with gastrointestinal issues, it can be hard to diagnose problems without being able to see what’s going on inside. Luckily, there are ways to take a look
Read more
When you’re dealing with gastrointestinal issues, it can be hard to diagnose problems without being able to see what’s going on inside. Luckily, there are ways to take a look
Read more
-
The Primary Role of a Gastroenterologist
posted: Nov. 08, 2023.
 Does something not feel right with your stomach? Our gastroenterologist is a specialist who dives deep into the world of your digestive system – stomach, intestines, liver, and more. Persistent
Read more
Does something not feel right with your stomach? Our gastroenterologist is a specialist who dives deep into the world of your digestive system – stomach, intestines, liver, and more. Persistent
Read more
-
Choosing Us as Your Gastroenterologist
posted: Oct. 10, 2023.
 Whether you’re dealing with stomach pain, or you want more information about preventive care like colon cancer screenings, it’s important that you find a gastroenterologist that you can trust and
Read more
Whether you’re dealing with stomach pain, or you want more information about preventive care like colon cancer screenings, it’s important that you find a gastroenterologist that you can trust and
Read more
-
Healthy Eating Habits for a Happy Gut
posted: Oct. 04, 2023.
 Healthy eating habits are crucial for your overall well-being. They provide your body with essential nutrients and support various bodily functions. Incorporating these habits into your life can lead to
Read more
Healthy eating habits are crucial for your overall well-being. They provide your body with essential nutrients and support various bodily functions. Incorporating these habits into your life can lead to
Read more
-
What Are the Symptoms of GERD?
posted: Sep. 15, 2023.
 When you eat certain foods or lay down too quickly after eating, you risk having acid reflux. This occurs when the esophagus doesn’t completely close to the stomach and acid
Read more
When you eat certain foods or lay down too quickly after eating, you risk having acid reflux. This occurs when the esophagus doesn’t completely close to the stomach and acid
Read more
-
Don't Ignore Abdominal Pain
posted: Sep. 01, 2023.
 Abdominal pain manifests as discomfort or ache in the area between your chest and pelvis. It can range from mild to severe, and symptoms like bloating, nausea, or cramping may
Read more
Abdominal pain manifests as discomfort or ache in the area between your chest and pelvis. It can range from mild to severe, and symptoms like bloating, nausea, or cramping may
Read more
